A patient’s age can greatly influence CPR and AED care, but it’s not the only factor. Children aren’t simply smaller versions of adults, their bodies react differently in emergencies. Recognizing whether someone is an infant, child, or adult helps rescuers act swiftly and choose the correct techniques for the best chance of survival. When determining “child” for CPR and AED purposes, we look at puberty as a guide, not just chronological age. Puberty brings real physical changes, such as growth and heart development, which affect how much force and what methods should be used during CPR.
For example, a 12-year-old who hasn’t started puberty may need child-specific care, while a younger individual showing early signs of puberty may require adult interventions. This approach ensures CPR matches the patient’s physical needs rather than just their age. In this guide, we’ll outline the age categories and explain how CPR and AED care differ for each, so you can respond confidently in any situation.
Why is it Important to define “Child” in CPR/AED Care
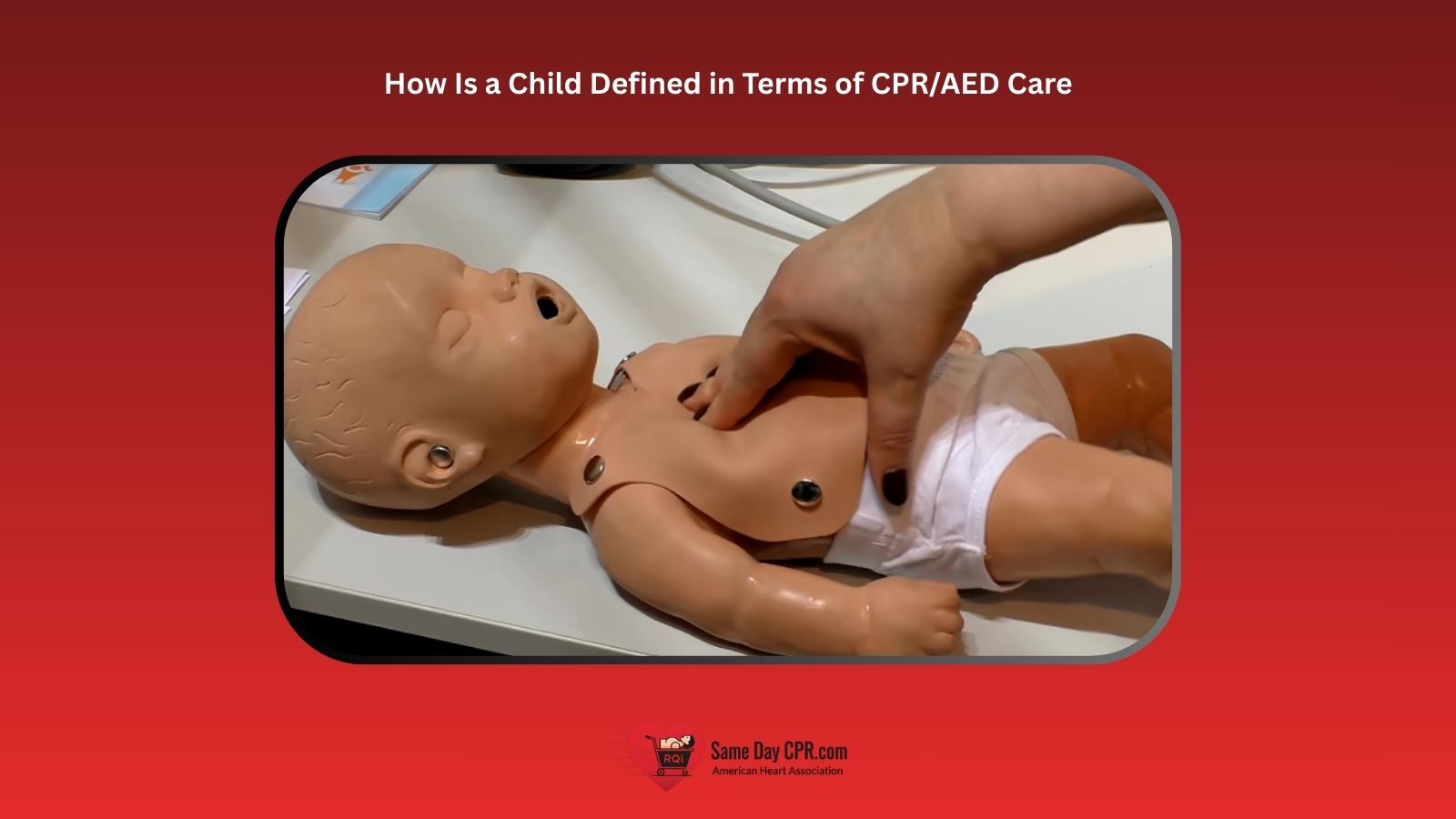
The primary purpose of defining a child is to ensure that chest compressions are performed with the correct force and that the AED is used properly. Using improper techniques can do more harm than good. Because a child’s body is smaller and their organs are still developing, they cannot tolerate the same level of compressive force as an adult, which is why knowing the target rate for chest compressions in children is so important.
How Child CPR Differs from Adult CPR
Child CPR is not the same as adult CPR because kids have smaller, more delicate bodies. Knowing the right way to help can make a big difference.
1. Proper Compression Depth and Technique for Children
- Adult: For adults, press down at least 2 inches on the chest using both hands.
- Child: For children, compress the chest about 2 inches or 5 centimeters, using one or two hands based on the child’s size.
2. Compression-to-Breath Ratio Adjustments
- Adult: For adults, the compression-to-breath ratio stays at 30 compressions to 2 breaths, no matter how many rescuers are present.
- Child: For children, a single rescuer should use a 30 to 2 ratio, but if there are two rescuers, the ratio changes to 15 compressions and 2 breaths.
3. Correct AED Pad Placement for Pediatric Patients
- Adult: For adults, place the AED pads on the upper right chest and the lower left side.
- Child: For children under 8 years or weighing less than 55 pounds (25 kg), use pediatric AED pads and place them on the chest and back in an anterior-posterior position.
Using an AED with Children: Key Considerations
Applying an AED to a child involves specific precautions and procedures to make sure it’s both safe and effective. Here’s what you should know.
1. Pediatric-specific AED pads
Pediatric AED pads are made just for children and babies. They are smaller than adult pads and deliver a gentle shock that is safe for young hearts. Using the right pads helps the AED work better and increases a child’s chance of survival during a sudden heart emergency. It’s easy to attach them, and they guide you step by step, making the process less scary for anyone helping.
2. Modifying AED shocks for children
When a child needs an AED, the device can adjust the shock to match their size and heart rate. This means the energy is lower and safer for young bodies. The AED guides you clearly, so you don’t have to worry about guessing. Using the right setting helps protect the child and gives them the best chance to recover.
3. Step-by-step instructions for operating an AED on a child
- Power on the AED and listen carefully to the instructions it gives.
- Attach the pads to the child exactly as shown in the directions.
- Make sure everyone steps away from the child before the device delivers a shock.
- If the AED instructs, start CPR right after the shock and keep going until emergency responders take over.
4. Identifying the right situations to use an AED
You should use an AED for a child if they are unresponsive and not breathing normally. The device can help restart their heart and guide you through each step. Using it quickly can make a big difference, especially while waiting for emergency help to arrive. It’s safe, easy, and gives the child the best chance to recover.
Step-by-Step CPR for Children
CPR can save a child’s life when their heart or breathing suddenly stops. Here’s a simple step-by-step guide to help you act quickly and confidently.
Step 1: Assess Responsiveness
Before starting CPR, gently tap the child on the shoulder and call their name to see if they respond. Speak clearly and stay calm as you check for any signs of movement, sound, or reaction. If the child does not respond, immediately ask someone nearby to call emergency services while you prepare to begin CPR.
Step 2: Open the Child’s Airway
Carefully place the child on their back on a firm surface. Gently tilt their head back by lifting the chin with one hand and pushing down on the forehead with the other. This simple movement helps keep the airway open so air can flow more easily into the lungs.
Step 3: Check for Breathing
Look closely to see if the child’s chest is rising and falling. Listen near their mouth and nose for any sounds of breathing, and feel for air against your cheek. Take no more than ten seconds for this step, and if you do not see normal breathing, prepare to start CPR right away.
Step 4: Begin Chest Compressions
Place the heel of one hand in the center of the child’s chest, just below the nipple line. Press down hard and fast, about two inches deep, at a steady rhythm of about 100 to 120 compressions per minute. Allow the chest to fully rise between each push to keep blood moving through the body.
Step 5: Deliver Rescue Breaths
After every 30 compressions, give two rescue breaths. Gently pinch the child’s nose closed, cover their mouth with yours, and blow until you see the chest rise. Each breath should be smooth and last about one second, helping deliver oxygen to their lungs.
Step 6: Continue CPR
Keep repeating cycles of 30 compressions and 2 breaths without stopping. Do not give up unless the child starts breathing normally, emergency responders take over, or you are too exhausted to continue. Staying focused and persistent gives the child the best chance of survival.
Final Thoughts on Pediatric CPR and AED Use
In short, understanding how to define a child in CPR and AED care gives rescuers the confidence to respond quickly and safely in emergencies. By using the right techniques, such as adjusting compression depth, changing the compression-to-breath ratio, or applying pediatric pads, you help protect a child’s body and give them the best chance to recover. Remember, it’s not just about age; it’s about recognizing physical development and responding in ways that match their needs. With this knowledge, you can step in calmly and effectively, making a real difference when every second matters.
Ready to take your skills to the next level? Get certified with Same Day CPR! We offer American Heart Association (AHA) Gold Standard courses in CPR, BLS, ACLS, PALS, and First Aid. Complete the online portion at your convenience, then finish with a quick 30-minute hands-on session at one of our 60+ convenient locations. Your official AHA certification card is issued immediately. Don’t wait. Call or visit our website today to secure your spot and gain the confidence to save lives.