A heart attack, also known as a myocardial infarction (MI), happens when the blood flow that provides the heart muscle is suddenly blocked. Without oxygen-rich blood, part of the heart muscle begins to die. This makes heart attacks a true medical emergency. According to the AHA data from 2005 to 2014, the estimated annual incidence of heart attacks in the United States was 605,000 new attacks and 200,000 recurrent attacks. The average age at the first heart attack was 65.6 years for males and 72.0 years for females.
Understanding what a myocardial infarction is matters because it’s one of the leading causes of death worldwide, yet many people don’t recognize the early warning signs. Knowing what’s happening in the body, what symptoms look like, and how to respond can literally save a life, whether it’s your own or someone else’s.
It’s also important to clear up a common confusion: a heart attack is not the same as cardiac arrest.
- A heart attack is a circulation problem; a blocked artery limits blood flow to the heart muscle.
- Cardiac arrest, on the other hand, is an electrical problem; the heart suddenly stops beating effectively. A heart attack can lead to cardiac arrest, but they are different conditions that require different responses.
Types of Heart Attack
A heart attack can show up in different ways, and each type affects the heart in its own way. Understanding these differences helps you recognize the signs and know why fast care truly matters.
1. STEMI (ST-Segment Elevation Myocardial Infarction)
A STEMI is the most serious type of myocardial infarction. It happens when a major coronary artery is completely blocked. With no blood reaching the affected area, the heart muscle begins to die quickly. On an ECG, this shows up as a clear “ST-segment elevation,” which is where the name comes from.
Key points:
- Caused by a full blockage.
- Requires immediate treatment, usually angioplasty/stenting or clot-busting medication.
- High risk of complications if not treated quickly.
2. NSTEMI (Non-ST-Segment Elevation Myocardial Infarction)
A NSTEMI occurs when a coronary artery is partially blocked. Blood flow is reduced, but not entirely cut off. Heart muscle damage still occurs, but typically not as extensively as with a STEMI. An ECG does not show ST-segment elevation, but blood tests (like troponin) reveal heart damage.
Key points:
- Partial blockage of a coronary artery.
- Still a medical emergency.
- Often treated with medications, followed by angiography and possible stenting.
Causes of Heart Attack
A heart attack happens when blood can’t reach part of the heart muscle, and the most common reason is a blocked coronary artery. While coronary artery disease is the leading cause, several less common conditions can trigger a myocardial infarction even in people without significant plaque buildup.
1. Coronary Artery Disease (Primary Cause)
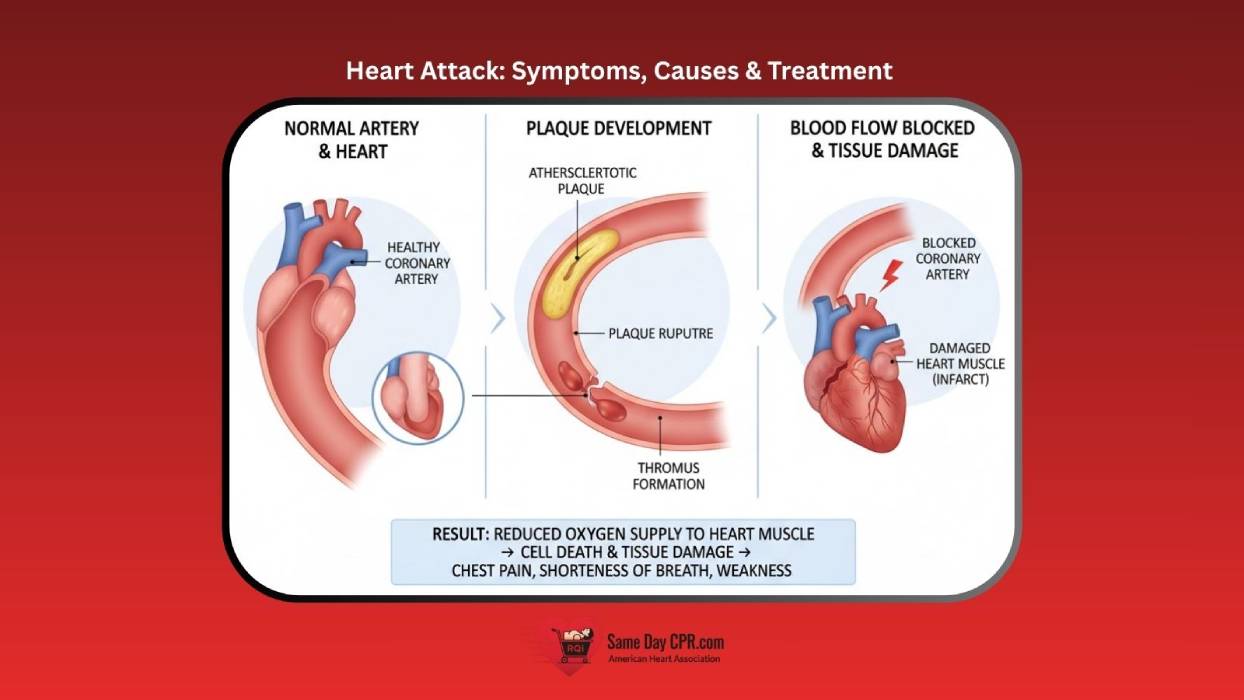
Coronary artery disease (CAD) is responsible for the vast majority of heart attacks. It develops slowly over time as fatty deposits, cholesterol, and other substances form a sticky buildup called plaque inside the artery walls, a process known as atherosclerosis.
Over time, this plaque narrows the arteries and restricts blood flow. A myocardial infarction usually occurs when:
- Plaque ruptures: A crack or break forms in the plaque.
- A blood clot forms: The body tries to repair the rupture, causing a clot that suddenly blocks the artery.
When that artery becomes fully blocked, the heart muscle downstream is starved of oxygen, leading to a heart attack.
2. Other Less Common Causes
Some heart attacks happen for reasons people don’t always expect. These less common causes still place serious stress on the heart and deserve attention.
2a. Coronary Artery Spasm
A temporary tightening of a coronary artery can sharply reduce blood flow. This spasm may occur in people with or without plaque buildup and can be triggered by stress, smoking, cold exposure, or certain medications.
2b. Spontaneous Coronary Artery Dissection (SCAD)
SCAD happens when a tear forms in the wall of a coronary artery. Blood flows into the tear, causing a blockage. This condition is more common in younger women and can occur without traditional risk factors.
2c. Drug-Induced Causes
Stimulant drugs, especially cocaine and methamphetamine, can trigger severe vessel spasm, high blood pressure, or abnormal heart rhythms, all of which can lead to a heart attack.
Risk Factors of Heart Attack
While heart attacks can occur at any age, middle-aged men and women experience high rates, and the risk rises with age, especially after menopause for women. However, there is a concerning trend of increasing heart attacks among younger adults, particularly those under 50, due to factors like obesity, diabetes, smoking, high blood pressure, and high cholesterol. This trend makes it even more important to understand the factors that can increase your risk.
Some risk factors are completely out of your control, while others can be improved through lifestyle changes, medication, or both. Understanding these risks helps people take meaningful steps toward prevention.
1. Modifiable Risk Factors
These are the risk factors you can influence. Improving them can dramatically lower your chance of experiencing a heart attack.
- High-Blood Pressure (Hypertension): Chronic high blood pressure puts stress on artery walls, making them more likely to develop plaque and rupture.
- High Cholesterol: Excess LDL (“bad”) cholesterol contributes to plaque formation inside coronary arteries, while low HDL (“good”) cholesterol can make the problem worse.
- Smoking: Smoking damages blood vessels, reduces oxygen supply, and accelerates plaque buildup. Even light or occasional smoking increases risk.
- Diabetes: High blood sugar damages blood vessels over time and is strongly linked to accelerated atherosclerosis.
- Obesity: Excess body weight, especially around the abdomen, raises the risk of high blood pressure, diabetes, and high cholesterol, all major contributors to heart attacks.
- Unhealthy Diet: Eating a diet high in saturated fats, trans fats, added sugars, and sodium increases the risk of heart disease.
- Excessive Alcohol Use: Extreme alcohol intake can cause a heart attack by raising blood pressure, damaging the heart muscle, and causing irregular heartbeats.
- Stress: Stress can trigger a myocardial infarction by increasing heart rate and blood pressure, releasing hormones that constrict blood vessels, and contributing to inflammation and plaque buildup.
2. Non-Modifiable Risk Factors
These are the risk factors you can’t change, but knowing them can help you stay proactive about your heart health.
- Age: The risk of a heart attack increases as you get older. With time, arteries naturally become stiffer and more prone to plaque buildup.
- Family History: Having a close relative, such as a parent or sibling, who developed heart disease early (typically before age 55 for men and 65 for women) significantly raises your risk.
- Sex / Biological Factors: Men generally face a higher risk at a younger age, while women’s risk increases after menopause. Hormonal differences, body fat distribution, and biological factors all play a role.
Signs and Symptoms of Heart Attack
A heart attack can start quietly, so it’s important to notice when your body feels “off” in a new or unusual way. Paying attention to these early signals can help you act fast and get the care you need.
- Chest Pain: You might feel pressure or tightness in the center of your chest that doesn’t go away. It can come on suddenly or build over time, making you stop and take notice.
- Fatigue: A myocardial infarction can leave you feeling unusually tired, even if you haven’t done much. This exhaustion may feel heavy and hard to shake off.
- Nausea: Some people feel sick to their stomach as their heart struggles. It can come with discomfort that makes you want to sit down and stay still.
- Heartburn or Indigestion: A burning or sour feeling in your upper body can sometimes be a warning sign. It may feel like common indigestion, but it doesn’t improve the way it normally would.
- Shortness of Breath: You may feel like you can’t catch your breath, even while resting. This can make simple movements feel harder than usual.
- Cold Sweat (Diaphoresis): Your body might break out in a sudden, clammy sweat for no clear reason. This can leave you feeling shaky as your heart works under stress.
Diagnosis of Heart Attack
Doctors use several tools to quickly check how your heart is doing when a myocardial infarction is suspected. These tests help them spot problems early so they can guide you toward the right treatment.
- ECG/EKG (Electrocardiogram): This test records your heart’s electrical activity to show if it’s beating normally. It helps doctors spot changes that may signal a blockage or heart damage.
- Blood Test: A simple blood draw can reveal proteins that appear when the heart is injured. These results give doctors a clear picture of what’s happening inside your body.
- Echocardiogram (Echo): This test uses sound waves to create images of your heart in motion. It lets doctors see how well your heart pumps and if any areas are not moving as they should.
- Chest X-ray: A quick image of your chest helps doctors check your heart’s size and shape. It also shows whether your lungs are affected by fluid or other changes.
- Chest Catheterization: During this test, a thin tube is gently guided into your heart to look for narrowed or blocked vessels. It also gives doctors a clear view to plan the best treatment for you.
- Stress Test: This test shows how your heart performs during activity by tracking its rhythm and blood flow. It helps doctors understand how your heart responds when it works a little harder.
Treatment of Heart Attack
Treating a heart attack starts with quick care to open blocked vessels and protect the heart from further harm. Doctors use a mix of medicines and procedures to restore healthy blood flow and support recovery.
1. Medications
- Thrombolytics: These medicines help break apart clots that block blood flow to the heart. They work quickly to open the vessel and limit further damage.
- Aspirin and Anticoagulants: These drugs make the blood less likely to clot and help keep vessels open. They support healthy flow while doctors continue your care.
- Nitroglycerin: This medicine relaxes and widens blood vessels to improve circulation. It can ease chest discomfort and help the heart work with less strain.
- Pain Medication: These medicines ease discomfort and help you feel calmer during treatment. They support your comfort while doctors focus on your heart.
2. Procedures
- Angioplasty and Stenting: Doctors guide a small balloon into the blocked vessel and gently open it. A tiny mesh tube called a stent is then placed to keep the vessel open and improve blood flow.
- Coronary Artery Bypass Grafting CABG: Surgeons create a new path for blood to move around a blocked vessel. This helps restore a steady flow to the heart and supports long-term recovery.
Complications of Heart Attack
A heart attack can lead to problems that affect how well the heart works, both right away and later on. Understanding these risks helps you know what to watch for and when to seek medical care.
1. Immediate and Serious Complications
- Cardiogenic Shock: This happens when the heart becomes too weak to pump enough blood to the body. It can cause dizziness, confusion, and severe trouble breathing as circulation drops.
- Arrhythmias: A heart attack can upset the heart’s rhythm, making it beat too fast, too slow, or unevenly. These changes can feel like fluttering, pounding, or pauses in your chest.
- Heart Rupture: In rare cases, damaged heart tissue can tear, leading to a sudden and dangerous drop in function. This requires immediate medical care to protect your life.
2. Other Potential Complications
- Pericarditis: The lining around the heart can become irritated after a heart attack. This may cause sharp chest discomfort that feels worse when you breathe deeply or lie down.
- Ventricular Septal Defect (VSD): A tear can form between the heart’s lower chambers after severe damage. This creates abnormal blood flow and requires urgent treatment to stabilize your heart.
- Heart Failure: A weakened heart muscle may struggle to pump enough blood to meet your body’s needs. This can lead to swelling, tiredness, and shortness of breath over time.
- Stroke: A clot or reduced blood flow during a myocardial infarction can affect the brain. This may cause sudden numbness, trouble speaking, or difficulty understanding simple actions.
Long-Term Management and Recovery
Long-term recovery focuses on helping your heart stay strong and lowering the chance of another attack. With steady habits, the right medicines, and guided support, you can build a healthier routine that fits your daily life.
- Lifestyle Changes: Healthy habits like balanced eating, regular movement, and quitting smoking help your heart work better each day. Small, steady choices can make a big difference in your long-term well-being.
- Medications: Your doctor may prescribe medicines to protect your heart, lower your risk, and manage symptoms. Taking them as directed helps keep your heart stable and supports your recovery.
- Cardiac Rehabilitation: This program offers supervised exercise, education, and support to help you feel stronger over time. It also teaches you how to care for your heart and build confidence in daily activities.
How to Prevent a Heart Attack
Preventing a myocardial infarction starts with everyday choices that keep your heart strong. Small steps add up, and with the right habits and care, you can lower your risk and stay healthier over time.
- Follow a Healthy Lifestyle: Eating balanced meals, staying active, and avoiding smoking help protect your heart every day. These simple habits strengthen your body and support long-term health.
- Manage Other Health Conditions: Keeping conditions like high blood pressure, diabetes, and cholesterol under control reduces extra strain on your heart. Regular check-ups and healthy routines make these goals easier to reach.
- Take Medications as Prescribed: If your doctor prescribes medicine, take it consistently to help lower your risk and maintain steady heart function. Staying on track with your treatment plan supports your overall well-being.
Protecting Your Heart Starts with Awareness
In short, a heart attack is a serious event, but understanding what causes it and how to respond can make a real difference. When you know the signs, you’re better prepared to get help quickly and protect your health. Small steps like eating well, staying active, and following your care plan can strengthen your heart over time. With the right knowledge and support, you can face this challenge with confidence and make choices that lead to a healthier, safer future.