When a pregnant person suddenly collapses, it can feel overwhelming, especially if you are the one trying to help. Cardiac arrest is serious, but knowing what to do right away can save lives. You are wondering if it is safe to use an AED (automated external defibrillator) on a pregnant woman or not. The answer is yes, you can absolutely use an AED on a pregnant woman, and doing so can help save two lives at once. Many people feel unsure or worry about hurting the baby, but an AED is safe and designed to restore a normal heart rhythm during a sudden emergency. Being pregnant doesn’t change how the AED works or what you should do. What matters most is acting quickly, staying calm, and giving the mother the best chance at recovery. When her heart is supported, the baby is protected, too.
Also, Read: What Are Some of the Special Considerations When Using an AED
Why an AED Is Safe During Pregnancy
An AED can be safely used on a pregnant patient during a cardiac arrest because the primary concern is restoring maternal circulation, which is critical for both the mother and the fetus. Key points include:
1. Electric Shock Does Not Harm the Fetus Directly
- The electrical current from an AED travels through the maternal chest to the heart.
- The current does not concentrate in the uterus, so the fetus is largely protected from the shock.
2. Maternal Survival is the Priority
- Restoring a normal heart rhythm in the mother is the most effective way to ensure fetal survival.
- Delaying defibrillation due to pregnancy concerns can be fatal for both mother and child.
3. Standard AED Protocol Applies
- Pad placement may be slightly adjusted if needed to avoid the enlarged uterus (e.g., anterior-posterior placement if the abdomen is obstructed), but the shock energy remains the same.
- Follow standard AED instructions, turn it on, attach pads, and allow it to analyze and deliver shocks if advised.
4. No Evidence of Harm from AED Use
- Clinical experience and case reports show that defibrillation during pregnancy is safe and life-saving.
Bottom line: AED use during pregnancy is safe and essential. The risk of not using it far outweighs any theoretical risk to the fetus.
When to Use an AED
An AED should be used on a pregnant woman any time she is unresponsive and not breathing normally. When the heart stops, both the mom and baby can lose oxygen fast.
1. Unresponsive and Not Breathing Normally
If the woman does not respond when you tap and talk to her, and her breathing is absent, gasping, or irregular, you should assume cardiac arrest. Do not wait to see if she “comes around.” Immediate action is critical.
2. Signs of Cardiac Arrest In a Pregnant Woman
Signs of cardiac arrest in a pregnant woman include sudden loss of consciousness, lack of breathing, and no pulse, but some warning signs, like chest pain, dizziness, or trouble breathing, might look like normal pregnancy changes, but they can also mean something serious. Other warning signs include extreme fatigue, a rapid or irregular heartbeat, fainting, nausea, and swelling in the hands or feet. Look for:
- No normal breathing
- No movement or response to touch
- Gasping or agonal breaths
- Sudden collapse
Note: If any of these signs are present, call 911, start CPR, and bring an AED as quickly as possible. Also, understand what is recommended to minimize interruptions in compressions when using an AED.
3. Importance of Quick Action
During cardiac arrest, oxygen stops flowing to both the mother’s brain and the baby.
- Brain damage can begin in 4-6 minutes without oxygen.
- The fetus loses oxygen even faster because it depends entirely on the mother’s circulation.
Using an AED promptly gives the best chance of restoring blood flow before irreversible harm occurs. The faster you act, the better the outcome for both mother and baby.
Step-by-Step: How to Use an AED on a Pregnant Woman
Step 1: Check for Response and Call Emergency Services: Assess whether the woman is responsive and breathing normally. If she is not, immediately call emergency services, inform them that she is pregnant, and request an AED.
Step 2: Begin CPR (cardiopulmonary resuscitation): Begin CPR by placing the woman flat on her back and starting high-quality chest compressions right away at a rate of 100 to 120 per minute and a depth of at least 2 inches, with your hands positioned slightly higher on the sternum. If you are trained, give 2 rescue breaths after every 30 compressions; if not, continue with hands-only CPR while knowing when to stop pushing on the victim’s chest during hands-only CPR, which helps guide your actions and keeps care consistent.
Step 3: Position for Blood Flow (Manual Left Uterine Displacement): For a visibly pregnant woman, a bystander should gently push the uterus to her left or place a rolled item under her right hip to create a left tilt. This helps improve circulation.
Step 4: Turn on the AED and Follow Prompts: Turn on the AED and follow prompts. Once the AED arrives, turn it on and follow its voice or visual instructions.
Step 5: Attach Pads: Expose the woman’s bare chest, removing any clothing or metal jewelry. Place the AED pads on her dry skin in the standard adult position: one on the upper right side of her chest (below the collarbone) and the other on the lower left side (a few inches below the armpit).
Step 6: Allow the AED to Analyze the Rhythm: Ensure no one is touching the woman’s body and loudly state “CLEAR!”. This step is essential, and you can learn more in our guide on: When should you clear the victim while operating the AED. Once everyone is clear, the AED will automatically analyze her heart rhythm.
Step 7: Deliver the Shock If Advised: If the AED advises a shock, ensure everyone is still clear of the patient. Press the flashing shock button when instructed (fully automatic AEDs will deliver the shock automatically after the “clear” warning).
Step 8: Immediately Resume CPR: After the shock is delivered (or if no shock is advised), immediately resume high-quality CPR, starting with chest compressions, for two minutes. Follow any further prompts from the AED, which will reanalyze the rhythm periodically.
Step 9: Place in Recovery Position in Conscious: If the woman regains consciousness and begins breathing normally, stop CPR but leave the AED pads on. Carefully roll her onto her left side to improve blood flow to the heart and fetus until emergency services take over.
Common Facts and Myths (Debunked)
When someone collapses during pregnancy, bystanders often hesitate, usually because of fear. But in a cardiac arrest, hesitation is far more dangerous than action. Here are three of the most common myths about using an AED on a pregnant woman, and the facts that debunk them.
- Myth: “You shouldn’t use an AED on a pregnant woman because it could harm the baby.”
- Fact: Using an AED is safe and necessary. The best way to protect the baby is to save the mother’s life first.
- Myth: “AED pads need to be placed in different spots on a pregnant woman.”
- Fact: AED pads are placed in the same standard positions, one on the upper right chest and one on the lower left side. No special placement is required.
- Myth: “The shock from an AED can cause pregnancy complications.”
- Fact: The AED’s shock goes through the mother’s chest only; it won’t reach the baby. Not using an AED when needed is far more dangerous.
Challenges While Performing an AED in Pregnant Women
1. Physical and Placement Challenges
Proper AED pad placement is vital for success. Rescuers need to navigate specific physical challenges to ensure the electricity effectively reaches the heart without causing injury.
1a. Breast Tissue
Proper AED pad placement involves avoiding breast tissue to ensure the electrical current effectively crosses the heart. This may require placing pads slightly differently than standard placement, for example, using an anterior/lateral position.
1b. Jewellery and Piercing
Metallic objects can interfere with the electrical current and potentially cause burns. Pads should not be placed directly over any jewelry or piercings, but these items do not need to be removed if they are not in the way.
1c. Medication Patches
Transdermal medication patches (e.g., nitroglycerin) must be removed, using gloves, before applying AED pads to prevent interference with the shock delivery and potential burns.
2. Physiological Challenges
A woman’s body changes significantly during pregnancy, which affects emergency care. Recognizing these physiological differences helps manage risks during resuscitation.
2a. Aspiration Risk
Pregnant women have an increased risk of regurgitation and aspiration (inhaling stomach contents into the lungs) due to physiological changes. Head positioning should be managed accordingly during resuscitation efforts.
2b. Airway Challenges
Hormonal and anatomical changes during pregnancy can make airway management and intubation more difficult.
2c. Increased Oxygen Demand
Pregnant women have a higher baseline oxygen demand, which means they desaturate (lose oxygen saturation) more quickly during cardiac arrest, making prompt and effective ventilation critical.
3. Emotional and Psychological Challenges
Emotional barriers are significant and can lead to dangerous delays in treatment. Understanding these psychological factors empowers bystanders to act without hesitation.
3a. Fear of Causing Harm
Bystanders and even medical professionals may hesitate to use an AED or perform full CPR due to a misconception that the electrical shock will harm the fetus. Medical consensus strongly supports that the risk of doing nothing is far greater than any potential risk from the AED.
3b. Hesitation to Expose the Body
Cultural or personal modesty can lead to hesitation in exposing the patient’s chest for proper pad placement. Rescuers should prioritize immediate life-saving action.
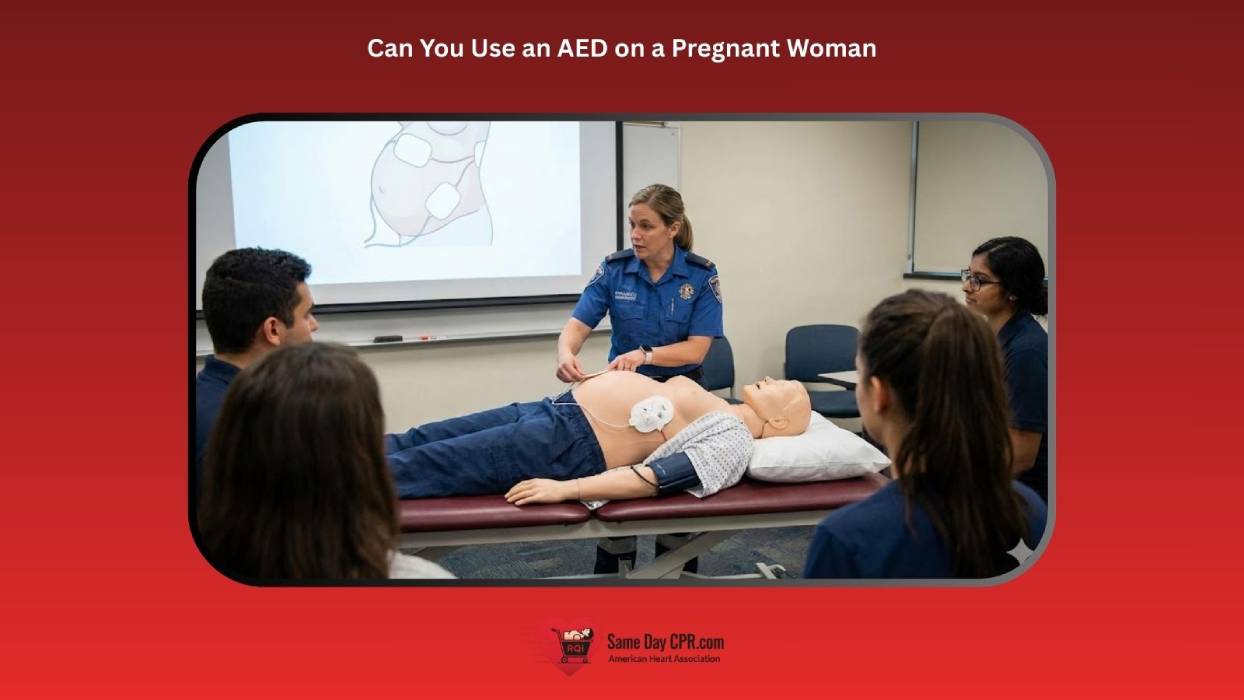
3c. Lack of Training with Female Manikins
Rescuers may have limited experience practicing CPR and AED use on manikins that accurately represent female anatomy, potentially leading to uncertainty in real-life scenarios involving women (pregnant or otherwise). This gap in training also connects to a broader issue: women are less likely to receive bystander CPR and AED, as hesitation often stems from discomfort or fear of doing something wrong.
When to Stop Using the AED
You should stop using the AED and performing CPR under the following circumstances:
1. Signs of Life Return
If the woman starts breathing, moving, or regains consciousness, stop CPR. Place her gently in the recovery position (on her left side) to improve blood flow to her heart and the baby, but leave the AED pads attached for monitoring in case she goes back into cardiac arrest.
2. Emergency Medical Services (EMS) Arrives and Takes Over
Continue all life-saving efforts until trained medical professionals reach the scene and physically relieve you of care.
3. A Rescuer Is Too Exhausted to Continue
High-quality CPR is physically demanding. If you are alone and become too tired to provide effective compressions, it is acceptable to stop. If others are present, switch rescuers every two minutes without delay to maintain continuous, high-quality CPR.
4. The Scene Becomes Unsafe
Personal safety is paramount. If the environment becomes dangerous (e.g., fire, traffic, structural collapse), move the patient to a safe area before resuming care or stop entirely if moving her is impossible.
Note: The AED itself provides voice or visual prompts to guide you and will instruct you to continue CPR or deliver a shock as needed. The device determines if a shockable rhythm is present and will not shock the patient unnecessarily. Therefore, you should never stop simply because you believe the AED should, unless the scenarios above are met.
Post-Resuscitation Management in Pregnancy
After successful resuscitation or when emergency medical services arrive, care transitions from immediate life-saving efforts to stabilization and specialized monitoring for both the mother and the fetus. The goals are to prevent recurrence of cardiac arrest, identify and treat underlying causes, and optimize maternal and fetal outcomes.
1. Maternal Assessment and Stabilization
- Airway and Breathing: Ensure the airway is secure; continue supplemental oxygen and monitor oxygen saturation. Consider an advanced airway if not already done.
- Circulation: Monitor vital signs, maintain blood pressure (avoid hypotension), and establish intravenous or intraosseous access.
- Cardiac Monitoring: Continuous ECG monitoring to detect arrhythmias. Treat according to standard ACLS guidelines adapted for pregnancy.
- Identify Reversible Causes (Hs & Ts): Hypoxia, hypovolemia, acidosis, tension pneumothorax, tamponade, toxins, thrombosis, etc., which may have contributed to the arrest.
Also, Read: Reversible Causes of Cardiac Arrest H’s and T’s
2. Fetal Assessment
- Fetal Heart Rate Monitoring: Continuous fetal monitoring is recommended if the gestational age is viable (usually >20 weeks).
- Assess Fetal Well-Being: Look for signs of fetal distress that may require urgent obstetric intervention.
3. Ongoing Support
- Oxygenation and Ventilation: Maintain maternal oxygen saturation >94%.
- Fluids and Medications: Administer fluids cautiously; medications must be safe in pregnancy when possible.
- Temperature Management: Avoid hypothermia or hyperthermia, as both can affect maternal and fetal outcomes.
4. Obstetric Consultation
- Immediate Involvement: Notify obstetrics for assessment and potential delivery if maternal status does not stabilize or if the fetus is in distress.
- Perimortem Cesarean Section: Consider if maternal cardiac arrest occurs in late pregnancy and resuscitation is unsuccessful after 4–5 minutes.
5. Documentation and Handover
- Record details of the arrest, resuscitation efforts, medications, and maternal-fetal status.
- Provide a clear handover to the intensive care or obstetric team for continued monitoring and care.
This phase is critical because maternal stabilization directly impacts fetal survival, and early recognition of complications can save both lives.
Also, Read: ACLS In-Hospital Cardiac Arrest in Pregnancy Algorithm
Act Quickly, Save Both Mom and Baby
In summary, using an AED on a pregnant woman is both safe and crucial. Acting quickly can save the mother’s life and give the baby the best chance of survival. The steps are the same as with any adult, and the shock only targets the heart, not the baby. Knowing the signs of cardiac arrest, starting CPR immediately, and using the AED without hesitation can make a life-or-death difference. Staying calm, following the device prompts, and focusing on the mother’s care ensures the fastest response. With the right actions, you can provide powerful help when it matters most.