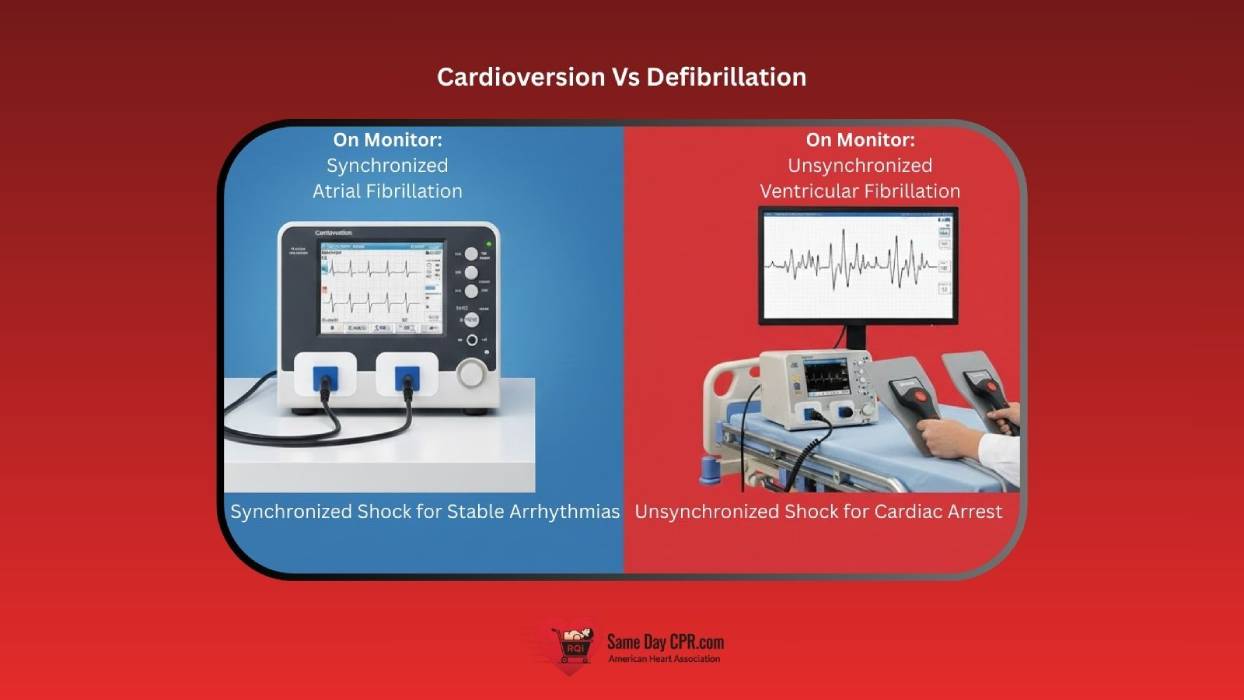
Cardioversion and defibrillation are both life-saving electrical therapies, but they are not interchangeable. Although they may look similar—pads on the chest and a shock delivered to the heart—using the wrong intervention at the wrong time can have serious and even fatal consequences.
Cardioversion is used when a patient still has a pulse, while defibrillation is reserved for cardiac arrest when no effective pulse is present. Using cardioversion on a patient in cardiac arrest can delay critical treatment, while delivering defibrillation to a patient who has a pulse can trigger dangerous arrhythmias or stop the heart altogether.
Understanding when to use cardioversion vs defibrillation is essential for safe, effective emergency care. The difference lies in timing, patient condition, synchronization, and energy delivery, all of which directly impact patient outcomes.
What Is Cardioversion
Cardioversion is a controlled electrical therapy used to correct certain abnormal heart rhythms, known as arrhythmias. It delivers a carefully timed electrical shock to the heart to restore a normal, organized rhythm. Unlike emergency shocks used during cardiac arrest, cardioversion is performed in a controlled setting using a cardiac monitor to synchronize the shock with the heart’s electrical activity.
This procedure is typically planned or semi-urgent rather than immediately life-saving. Cardioversion is commonly used when a patient has a pulse but is experiencing symptoms such as chest discomfort, shortness of breath, dizziness, or low blood pressure due to an abnormal rhythm. Because the patient is conscious in most cases, cardioversion is often performed with sedation to minimize discomfort while allowing clinicians to safely correct the rhythm.
1. Types of Cardioversion
There are two main ways to perform cardioversion, depending on the patient’s condition and the heart rhythm involved. One uses electricity, while the other relies on medication to restore a normal rhythm.
1a. Synchronized Electrical Cardioversion
- How It Works: A controlled electrical shock is delivered at a precise moment in the heart’s rhythm to reset electrical activity safely.
- When to Use: Used when a patient has a pulse and an unstable or symptomatic rhythm such as atrial fibrillation, atrial flutter, or SVT.
- Key Features:
- Shock is synchronized with the heart’s electrical cycle
- Lower energy levels than defibrillation
- Usually performed with sedation
1b. Pharmacologic (Chemical) Cardioversion
- How It Works: Medications are given to slow abnormal electrical signals and help the heart return to a normal rhythm.
- When to Use: Often chosen for stable patients or when electrical cardioversion is not immediately needed or available.
- Key Features:
- No electrical shock involved
- It may take minutes to hours to work
- Requires close monitoring for side effects
2. Rhythms Treated With Cardioversion
Cardioversion is used to correct organized abnormal heart rhythms when the patient still has a pulse. These rhythms respond well to controlled, synchronized therapy.
- Atrial Fibrillation: An irregular and often rapid rhythm that starts in the atria and can reduce effective blood flow.
- Atrial Flutter: A fast but more organized atrial rhythm that often responds quickly to synchronized cardioversion.
- Supraventricular Tachycardia SVT: A rapid rhythm originating above the ventricles that can cause palpitations, dizziness, or chest discomfort.
- Stable Ventricular Tachycardia With a Pulse: A dangerous ventricular rhythm where the patient remains conscious and perfusing, allowing for synchronized cardioversion rather than emergency defibrillation.
3. How Cardioversion Works
Cardioversion delivers an electrical shock that is synchronized with the R wave of the heart’s electrical cycle. This timing ensures the shock is released during a safe phase of ventricular depolarization, when the heart is least vulnerable to dangerous rhythm changes.
Synchronization prevents the R on T phenomenon, which can occur if a shock is delivered during the heart’s recovery phase. Delivering energy at the wrong moment can trigger ventricular fibrillation, so synchronized timing helps correct the rhythm without creating a more life-threatening arrhythmia.
What Is Defibrillation
Defibrillation is an emergency, life-saving treatment used when the heart is no longer pumping blood effectively. It delivers a powerful electrical shock to stop chaotic electrical activity and give the heart a chance to restart with a normal rhythm.
This therapy is used during cardiac arrest, when the patient has no pulse and is unresponsive. Defibrillation must be delivered quickly, often with an AED ( Automated External Defibrillator) or cardiac monitor, because every second without effective circulation reduces the chance of survival.
1. Types of Defibrillation
There are a few ways to deliver a defibrillation shock, depending on the situation and available equipment. Each method is designed to quickly stop chaotic heart rhythms and restore a normal rhythm.
1a. Manual Defibrillation
A trained clinician delivers a controlled shock using a cardiac monitor or defibrillator. The energy level and timing are set based on the patient’s rhythm.
1b. Automated External Defibrillator (AED)
An AED analyzes the heart rhythm and advises or delivers a shock automatically. It is designed for use by both healthcare providers and trained laypersons in emergencies, so it’s important to follow the special considerations for using an AED safely.
1c. Biphasic vs. Monophasic Defibrillation
- Biphasic: Delivers current in two directions, often requiring lower energy and causing less heart damage.
- Monophasic: Delivers current in a single direction, typically at higher energy levels.
2. Rhythms Treated With Defibrillation
Defibrillation is used for life-threatening heart rhythms that cause cardiac arrest and produce no effective pulse. These rhythms are chaotic and require an immediate, unsynchronized shock.
- Ventricular Fibrillation (VF): A disorganized rhythm where the ventricles quiver instead of pumping blood, leading to sudden cardiac arrest.
- Pulseless Ventricular Tachycardia (pVT): A rapid ventricular rhythm that produces no pulse and prevents effective circulation, requiring immediate defibrillation.
3. How Defibrillation Works
Defibrillation delivers an unsynchronized electrical shock to the heart without timing it to the cardiac cycle. Because there is no organized rhythm present, the shock is given immediately to avoid delays in life-saving care.
The goal is to stop chaotic electrical activity all at once so the heart’s natural pacemaker can regain control. By resetting the heart’s electrical system, defibrillation gives the best chance for a normal rhythm to return.
Side-by-Side Comparison: Cardioversion vs Defibrillation
This comparison highlights the critical differences between cardioversion and defibrillation and shows why choosing the correct intervention matters.
| Feature | Cardioversion | Defibrillation |
| Synchronization | Synchronized with the R wave | Unsynchronized |
| Indications | Unstable or symptomatic arrhythmias with a pulse | Cardiac arrest due to VF or pulseless VT |
| Rhythms Treated | Atrial fibrillation, atrial flutter, SVT, stable VT with pulse | Ventricular fibrillation, pulseless ventricular tachycardia |
| Energy Levels | Lower joules (typically 50–200 J) | Higher joules (typically 120–360 J) |
| Patient Status | Patient has a pulse, often conscious | No pulse, unresponsive |
Common Myths and Misconceptions
Even though cardioversion and defibrillation are widely used, several myths can confuse or delay proper care. Understanding the facts helps both healthcare providers and bystanders respond correctly in an emergency.
Myth 1: Defibrillation Restarts the Heart
– Many people think the shock “restarts” a stopped heart, but it actually stops disorganized electrical activity so the heart’s natural pacemaker can regain control.
Myth 2: Cardioversion Can Be Used During Cardiac Arrest
– Cardioversion requires a pulse, so it is not suitable for patients in cardiac arrest. Using it incorrectly can waste valuable time.
Myth 3: AEDs Can Be Used Without Any Training
– While AEDs are user-friendly, proper training ensures pads are placed correctly, the area is clear, and shocks are delivered safely.
Myth 4: Higher Energy Always Works Better
– More energy does not always improve outcomes and can increase the risk of heart damage, so following recommended joule settings is essential.
General Risks (Both Procedures)
- Blood Clots and Stroke: Irregular heart rhythms, such as atrial fibrillation, can allow clots to form. Delivering a shock might dislodge these clots, which can lead to a stroke or pulmonary embolism.
- Skin Burns: Minor burns at the site of the paddles or pads are possible, especially with older equipment or improper placement. Modern biphasic devices and gel pads have reduced this risk.
- New Arrhythmias: Sometimes, the shock can trigger other abnormal heart rhythms that may require additional treatment.
- Heart Muscle Effects: High-energy shocks can temporarily weaken heart function or, in rare cases, cause minor heart muscle injury.
- Sedation-Related Issues: Patients may experience allergic reactions or side effects from anesthesia used during cardioversion.
1. Cardioversion-Specific Risks
- Recurrence of Rhythm: The abnormal rhythm can return after cardioversion, sometimes requiring repeat treatment.
- Slow Heartbeats or Pauses: The procedure may temporarily slow the heart or cause brief pauses in rhythm.
2. Defibrillation-Specific Risks
- Correct Indication is Crucial: Applying a shock to a patient without a life-threatening rhythm, like ventricular fibrillation, can actually trigger dangerous arrhythmias and stop the heart.
Management and Prevention
- Blood Thinners: Patients, especially those with AFib lasting more than 48 hours, often take anticoagulants before and after cardioversion to prevent clots.
- Transesophageal Echocardiography (TEE): A TEE can be performed to check for clots before cardioversion.
- Proper Technique: Using modern equipment and placing pads correctly helps minimize burns and other complications.
- Medications: Anti-arrhythmic drugs may be prescribed after the procedure to reduce the chance of rhythm recurrence.
ACLS and BLS Guidelines Overview
The American Heart Association (AHA) guidelines clearly differentiate between cardioversion and defibrillation based on the patient’s condition and the type of rhythm present. Cardioversion is recommended for patients with a pulse who have unstable or symptomatic arrhythmias, while defibrillation is used in cardiac arrest situations such as ventricular fibrillation or pulseless ventricular tachycardia.
Accurate rhythm recognition is essential in both ACLS and BLS protocols. Determining whether the rhythm is organized with a pulse or chaotic without a pulse ensures the correct intervention is delivered quickly, which can greatly improve patient outcomes.
AEDs and cardiac monitors are key components of these guidelines. AEDs enable both trained laypersons and healthcare providers to deliver timely shocks during emergencies, while monitors offer continuous rhythm assessment in clinical settings, guiding synchronized cardioversion or manual defibrillation as needed.
Safety Considerations and Best Practices
Using cardioversion or defibrillation can save lives, but it is important to follow safety steps. Paying attention to technique, communication, and monitoring keeps both the patient and team safe.
1. Pad Placement
Proper placement of defibrillator or cardioversion pads is crucial to ensure effective shock delivery and minimize the risk of burns or ineffective treatment. Follow manufacturer instructions and standard protocols for anterior-posterior or anterior-lateral positions.
2. Clear Communication During Shock Delivery
Always announce loudly and clearly before delivering a shock to ensure everyone is aware and no one is in contact with the patient or bed, and follow guidelines on when the rescuer operating the AED should clear the victim to maintain safety.
3. Monitoring and Post-Shock Care
After delivering a shock, continuously monitor the patient’s heart rhythm, blood pressure, and oxygen levels. Be ready to provide additional interventions, such as repeat shocks, medications, or advanced airway support, if needed.
Choosing the Right Shock at the Right Time
In summary, cardioversion and defibrillation both save lives, but they serve very different moments in care. Cardioversion helps fix certain abnormal rhythms when a pulse is present, while defibrillation treats cardiac arrest when the heart cannot pump blood. Knowing which one to use comes down to the patient’s condition and the rhythm on the monitor. When you understand this difference and act with confidence, you protect the patient, avoid harmful mistakes, and give the heart the best chance to recover.
For healthcare professionals and students looking to build confidence with these critical skills, Same Day CPR offers AHA ACLS, BLS, PALS, CPR, and First Aid certification. Complete the AHA online course included with registration, then visit one of our 60+ locations for a quick, in-person skills session that takes about 30 minutes. You’ll receive your official American Heart Association certification card immediately after completion.