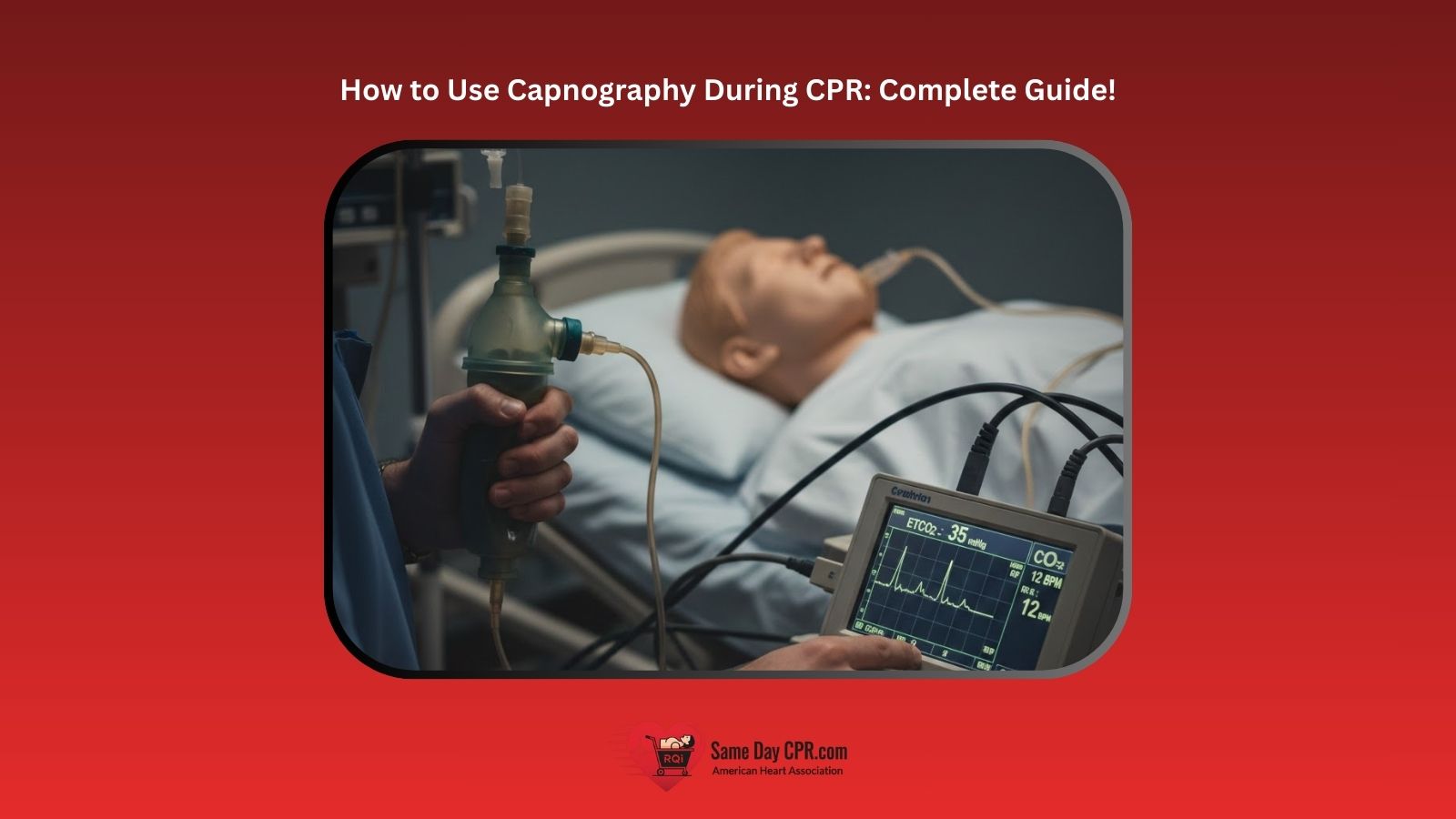
High-quality CPR isn’t just about pushing hard and fast, it’s about knowing whether your efforts are actually working. Capnography allows you to measure CPR effectiveness in real time by tracking end-tidal carbon dioxide (EtCO₂), giving immediate feedback on chest compressions, ventilation, and circulation during cardiac arrest.
Capnography is a non-invasive monitoring tool that measures the amount of carbon dioxide exhaled at the end of each breath. During CPR, EtCO₂ levels directly reflect cardiac output generated by chest compressions, making capnography one of the most reliable indicators of CPR quality and early return of spontaneous circulation (ROSC). For this reason, current Advanced Cardiac Life Support (ACLS) guidelines strongly recommend using continuous waveform capnography throughout resuscitation. When used correctly, capnography helps providers:
- Confirm proper airway placement
- Adjust chest compression depth and rate
- Detect ventilation problems
- Recognize ROSC earlier than pulse checks
Studies show that persistently low EtCO₂ values (below 10 mmHg) during CPR are associated with poor outcomes, while sustained readings above 20 mmHg significantly improve the likelihood of successful resuscitation.
This complete guide walks you step by step through how to use capnography during CPR, from setting up the equipment and interpreting waveforms to adjusting compressions and identifying ROSC, so you can deliver more effective, data-driven resuscitation when it matters most.
Why Capnography is Critical During CPR
Capnography is more than just a monitoring tool; it’s a critical guide during resuscitation. Its real-time feedback allows healthcare providers to make immediate adjustments, improving the effectiveness of CPR and patient outcomes. Here’s why it’s so important:
1. Real-Time Feedback on Chest Compression Quality
High-quality chest compressions are the cornerstone of effective CPR. Capnography provides instant feedback through ETCO₂ readings, helping clinicians assess compression effectiveness, while a chest compression feedback device monitors metrics like depth, rate, and recoil in real time to guide optimal performance.
- Compression depth and rate
- Adequacy of circulation generated by compressions
- Need for adjustment in technique
Low or dropping ETCO₂ values can indicate ineffective compressions, prompting immediate correction.
2. Early Detection of ROSC
A sudden rise in ETCO₂ during CPR often signals ROSC (Return of Spontaneous Circulation) before other vital signs are detectable. This early detection allows providers to quickly transition from compressions to post-resuscitation care, improving survival chances.
3. Identifying Ventilation Issues
Capnography helps detect ventilation problems, such as:
- Hyperventilation: ETCO₂ drops due to over-ventilation.
- Hypoventilation: ETCO₂ rises, indicating insufficient breathing support.
- Airway obstruction or leaks: Abnormal waveforms alert the team to issues with the airway or ET tube placement.
4. Enhancing Patient Outcomes
By providing continuous, actionable information, capnography ensures interventions are precise and timely, which contributes to:
- More effective CPR
- Faster recognition of ROSC
- Reduced complications from improper ventilation
- Overall improved survival rates
In summary, capnography turns CPR from a “blind” procedure into a data-driven, responsive process, enabling providers to make informed decisions in real time.
Choosing and Setting Up Capnography Equipment
Using capnography effectively during CPR begins with having the right equipment and setting it up correctly. Proper preparation ensures accurate readings and reliable feedback throughout resuscitation.
1. Choosing the Right Capnography Device
- Mainstream vs. Sidestream: Select based on patient type, airway device, and clinical setting.
- Mainstream: Best for real-time, immediate readings; ideal for intubated patients.
- Sidestream: Lightweight, versatile; suitable for transport or mask ventilation.
- Portability and Integration: Consider whether the device can easily integrate with existing monitors and ventilators.
- Battery Life and Durability: Ensure devices are fully charged and capable of continuous monitoring during prolonged resuscitation.
2. Placement of Sensors and ET Tube Connection
- Intubated Patients: Connect the sensor directly to the endotracheal tube (ET tube) between the tube and the ventilation circuit.
- Non-Intubated Patients: Use a mask adapter for sidestream sampling if bag-mask ventilation is required.
- Waveform Verification: Confirm a stable capnogram before starting compressions to ensure accurate monitoring.
3. Troubleshooting Common Device Issues
- Flatline or No Reading: Check sensor connection, tubing for kinks, or device calibration.
- Erratic Waveforms: Remove condensation from tubing or sensor, ensure secure airway placement.
- Low ETCO₂ Despite Effective CPR: Consider equipment malfunction, patient hypoperfusion, or technical interference.
4. Calibration and Maintenance Tips
- Calibration: Perform according to manufacturer instructions before use; some devices are pre-calibrated.
- Cleaning: Follow infection control guidelines, clean reusable sensors after each patient.
- Routine Maintenance: Inspect for damage, replace batteries or sampling lines regularly, and check software updates for digital devices.
By ensuring proper equipment selection, correct placement, and routine maintenance, providers can rely on capnography to deliver accurate, real-time feedback during CPR.
Step-by-Step Guide: Using Capnography During CPR
Capnography provides real-time feedback that can guide resuscitation efforts. Proper use ensures that chest compressions and ventilations are effective and helps detect the return of spontaneous circulation (ROSC) early. Here’s a step-by-step guide:
1. Connect the ET Tube or Mask to the Capnography
The first step is to connect the ET tube or mask to the capnography device. For intubated patients, attach the sensor directly between the ET tube and the ventilation circuit. For non-intubated patients, use a mask adapter with a sidestream device to sample exhaled CO₂. Make sure all connections are secure to prevent leaks that could affect the accuracy of the readings.
2. Confirm Waveform and Baseline ETCO₂
Next, confirm the waveform and establish a baseline EtCO₂. Before starting chest compressions, make sure the capnogram shows a clear, stable waveform. Record the baseline EtCO₂ to track changes throughout the resuscitation process.
3. Monitor Trends During Chest Compressions
During chest compressions, continuously monitor EtCO₂ values and the waveform shape. Steady readings indicate effective compressions, while consistently low values may signal inadequate circulation. Use this information to adjust compression depth and rate to optimize blood flow.
4. Adjust Compressions Based on Readings
Adjust chest compressions based on EtCO₂ readings. If the values drop significantly, check for poor compression quality, airway obstruction or disconnection, and hypoperfusion. Address any issues immediately to maintain effective CPR and ensure adequate circulation.
5. Recognize Signs of ROSC
Recognize signs of ROSC by watching for a sudden rise in EtCO₂, which often occurs before palpable pulses or changes in blood pressure. Detecting this early allows the team to transition smoothly from chest compressions to post-resuscitation care.
6. Integrating with Other Monitoring Tools
Integrate capnography with other monitoring tools for a complete view of the patient’s status. Combine EtCO₂ data with ECG monitoring to track rhythm changes, pulse oximetry to observe oxygen saturation trends, and blood pressure measurements when available. This integrated approach allows for more precise and timely interventions during resuscitation.
By following these steps, capnography becomes an essential guide during CPR, allowing clinicians to optimize compressions, detect ROSC early, and improve patient outcomes. To maximize effectiveness, it’s important to understand how you can achieve a high chest compression fraction.
Target EtCO₂ Values During CPR and What They Mean
Understanding numeric EtCO₂ targets allows providers to translate capnography data into immediate clinical action during resuscitation.
Target EtCO₂ Ranges During CPR
| EtCO₂ Value (mmHg) | What It Indicates | What to Do |
| < 10 mmHg | Inadequate cardiac output from compressions | Improve compression depth, rate, recoil; minimize pauses; switch compressors |
| 10–20 mmHg | Marginal or inconsistent CPR quality | Optimize compressions, reassess the airway and ventilation |
| ≥ 20 mmHg | High-quality CPR with effective circulation | Maintain current technique |
| Sudden rise to ≥ 35–40 mmHg | Likely ROSC | Stop compressions, check pulse, transition to post-ROSC care |
Key Clinical Takeaways
- Persistently low EtCO₂ (<10 mmHg) despite optimized CPR is associated with poor outcomes.
- Sustained EtCO₂ ≥20 mmHg significantly improves the likelihood of successful resuscitation.
- Abrupt increases in EtCO₂ often signal ROSC before pulses or blood pressure are detectable.
Capnography should be used to monitor trends, not isolated numbers, and always interpreted alongside ECG and clinical findings.
Adult vs Pediatric EtCO₂ Interpretation During CPR
While capnography principles are consistent across age groups, EtCO₂ values must be interpreted within the clinical context of adult and pediatric physiology.
1. Adult CPR
In adult CPR, EtCO₂ primarily reflects the cardiac output generated by chest compressions. Target values include a minimum of 10 mmHg, while readings at or above 20 mmHg indicate high-quality CPR. A sudden rise in EtCO₂ often strongly suggests the return of spontaneous circulation, allowing providers to recognize ROSC early and adjust care accordingly.
2. Pediatric CPR
In pediatric CPR, EtCO₂ values can be more variable because of smaller tidal volumes, faster respiratory rates, and respiratory-related causes of arrest. Slightly lower EtCO₂ readings may still be acceptable as long as the waveforms remain consistent, chest compressions are high quality, and ventilation rates are appropriate.
Key Pediatric Considerations
- Avoid hyperventilation, which can falsely lower EtCO₂.
- Focus on waveform quality and trends, not just numeric thresholds.
- Always interpret EtCO₂ alongside oxygenation, heart rate, and perfusion signs.
Common Challenges and How to Overcome Them
While capnography is a powerful tool during CPR, several challenges can affect accuracy and interpretation, especially in high-stress resuscitation scenarios. Understanding these issues helps providers respond quickly and maintain reliable monitoring.
1. Motion Artifacts During Chest Compressions
- Challenge: Continuous chest compressions can cause waveform distortion or fluctuating ETCO₂ readings.
- How to Overcome It:
- Focus on ETCO₂ trends, not single values.
- Ensure the sensor and airway connections are secure.
- Avoid unnecessary movement of the airway device during compressions.
2. Low Signal or Flatline Readings
- Challenge: No waveform or very low ETCO₂ readings can be alarming and may be mistaken for equipment failure or patient deterioration.
- How to Overcome It:
- Check for disconnected sensors or kinked sampling lines.
- Verify proper ET tube placement and mask seal.
- Assess compression quality and adjust depth or rate if needed.
- Confirm the device is powered on and functioning correctly.
3. Interference from Other Devices
- Challenge: Suctioning, defibrillation, or ventilator adjustments can temporarily disrupt capnography readings.
- How to Overcome It:
- Expect brief waveform changes during these interventions.
- Reassess the waveform immediately afterward to confirm accurate readings.
- Maintain clear communication among team members to minimize disruption.
Tips for Accurate Interpretation Under Stress
- Assign a designated team member to monitor capnography when possible.
- Watch for sudden changes in ETCO₂ rather than gradual fluctuations.
- Use capnography alongside ECG and clinical assessment, not in isolation.
- Practice interpreting waveforms during training simulations to build confidence.
By anticipating common challenges and knowing how to address them, healthcare providers can rely on capnography as a consistent and trustworthy guide during CPR, even in fast-paced, high-pressure situations.
Key Takeaways: Using Capnography to Optimize CPR
In short, using capnography during CPR gives you real-time information that makes every compression count. It helps you know if your compressions are effective, whether the patient is ventilating properly, and if circulation is returning. By watching trends and responding quickly to changes, you can provide smarter, faster care and improve the chances of survival. With practice, capnography becomes a reliable partner in guiding CPR, keeping you confident and focused when it matters most.
If you are looking to strengthen your skills further, Same Day CPR offers ACLS, BLS, PALS, CPR, and First Aid certification classes in Delaware, the District of Columbia, Georgia, Maryland, Missouri, New Jersey, New York, North Carolina, Pennsylvania, South Carolina, Texas, and Virginia. To learn more about these life-saving courses, call 888-840-5527, send an inquiry to info@samedaycpr.com, or visit one of our training centers.