ACLS Suspected Stroke Algorithm: Assessment and Treatment Guide
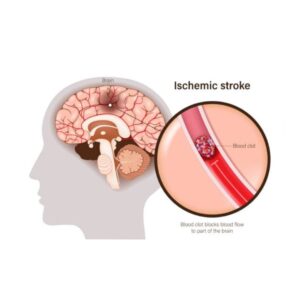
A stroke occurs when blood flow to part of the brain is cut off, quickly damaging brain cells and requiring fast medical action. According to the CDC, over 795,000 people in the U.S. experience a stroke annually, with about 87% being ischemic strokes caused by blocked blood vessels, stopping oxygen from reaching the brain.