Cardiac arrest happens when the heart suddenly stops beating properly, cutting off blood flow to the brain and other vital organs. Without immediate help, the person quickly loses consciousness and stops breathing. This is a true medical emergency that requires fast action to save a life. Many people confuse cardiac arrest with a heart attack, but they are not the same. A heart attack happens when blood flow to part of the heart is blocked, while cardiac arrest is when the heart stops working altogether. Knowing the difference and how to respond can make all the difference in an emergency.
Pathophysiology of Cardiac Arrest
Cardiac arrest occurs when the heart suddenly stops pumping blood effectively, leading to a cessation of circulation. Without immediate intervention, this results in loss of oxygen delivery to vital organs, especially the brain, causing irreversible damage within minutes.
Key Mechanisms
1. Electrical Dysfunction
- Most commonly, cardiac arrest is caused by ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT).
- These arrhythmias prevent coordinated contractions, stopping effective blood flow.
2. Mechanical Dysfunction
- The heart may fail to pump due to severe myocardial infarction, cardiomyopathy, or massive pulmonary embolism.
- Even if electrical activity persists, mechanical pumping is inadequate—this is called pulseless electrical activity (PEA).
3. Respiratory or Metabolic Causes
- Hypoxia, acidosis, electrolyte imbalances (e.g., hyperkalemia), or drug toxicity can disrupt cardiac function, triggering arrest.
4. Circulatory Collapse
- Severe blood loss or shock states reduce preload and perfusion, contributing to arrest.
Cellular and Organ Effects
- Brain: Neurons are highly sensitive to oxygen deprivation; irreversible injury can occur within 4-6 minutes.
- Heart: Ischemia worsens arrhythmias and reduces the chances of successful resuscitation.
- Other Organs: Kidneys and liver suffer early hypoperfusion, impacting recovery post-arrest.
Cardiac arrest is a final common pathway resulting from electrical, mechanical, respiratory, or metabolic failure. Understanding the pathophysiology is critical because it guides both immediate resuscitation and post-arrest care.
Causes and Risk Factors of Cardiac Arrest
Causes
Cardiac arrest is caused by irregular heart rhythms (arrhythmias) often stemming from underlying heart conditions like coronary artery disease, cardiomyopathy, and congenital heart defects.
- Coronary Artery Disease (CAD): When the arteries that supply blood to the heart get clogged, the heart can’t get enough oxygen. This can trigger a heart attack and sometimes stop the heart completely.
- Irregular Heart Rhythm (Arrhythmias): Sometimes the heart beats too fast, too slow, or in an uneven pattern. This can make it hard for the heart to pump blood properly and may lead to sudden cardiac arrest.
- Heart Muscle Abnormalities (Cardiomyopathy): Weak or damaged heart muscles struggle to pump blood efficiently. Over time, this can make the heart fail suddenly and cause cardiac arrest.
- Structural Heart Defects: Some people are born with problems with the heart’s shape or its valves. These defects can disrupt blood flow and increase the risk of the heart stopping.
- Other Medical Conditions: Certain illnesses like diabetes, high blood pressure, or severe infections put extra stress on the heart. This added strain can sometimes lead to sudden cardiac arrest.
Risks
Major risk factors include traditional ones like high blood pressure, high cholesterol, diabetes, obesity, and smoking, as well as lifestyle and other medical factors like electrolyte imbalances, certain medications, and strenuous physical exertion.
- Smoking: It damages the heart and blood vessels, making it harder for your heart to get enough oxygen. Quitting helps your heart recover and lowers your risk of cardiac arrest.
- Diabetes: High blood sugar weakens blood vessels and can harm the heart over time. Keeping diabetes under control protects your heart and improves overall health.
- Obesity or Physical Inactivity: Carrying extra weight and not staying active puts extra stress on the heart. Regular movement and a balanced diet can greatly reduce your risk.
- Family History of Sudden Cardiac Death: If heart problems run in your family, your own risk may be higher. Knowing your family’s heart health helps you take early steps to stay protected.
- Substance Abuse: Using drugs like cocaine or amphetamines can cause dangerous heart rhythms. Avoiding these substances keeps your heart’s rhythm strong and steady.
- Chronic Kidney Disease: When the kidneys don’t work well, it can upset your body’s balance and strain the heart. Managing kidney health helps lower your chance of cardiac arrest.
Early Recognition and Warning Signs
Recognizing the early signs of cardiac arrest can help you act quickly and save a life. Knowing what to look for gives you the confidence to respond when someone’s heart suddenly stops.
- Chest Pain or Discomfort Before Collapse: Some people may feel heavy pressure or pain in their chest just before collapsing. It’s the heart’s way of warning that something serious is about to happen.
- Sudden Dizziness or Fainting: Feeling lightheaded or losing consciousness out of nowhere can be an early sign that blood flow to the brain is dropping fast. Recognizing this early and calling for help can prevent full cardiac arrest.
- Sudden Collapse: A person may suddenly fall to the ground without any warning. This is one of the first and most obvious signs that the heart has stopped working properly. Acting quickly at this moment can truly make the difference between life and death.
- No Response: If you tap the person and they don’t move, open their eyes, or speak, it means they are unresponsive. This shows that their brain isn’t getting enough oxygen, and immediate help is needed.
- No Normal Breathing: When someone isn’t breathing or only gasping weakly, it’s a strong signal of cardiac arrest. Checking their breathing right away helps you know if CPR (cardiopulmonary resuscitation) should begin.
- No Pulse: If there’s no pulse, the heart has stopped pumping blood through the body. Quickly checking for a pulse helps confirm cardiac arrest so you can start life-saving steps without delay.
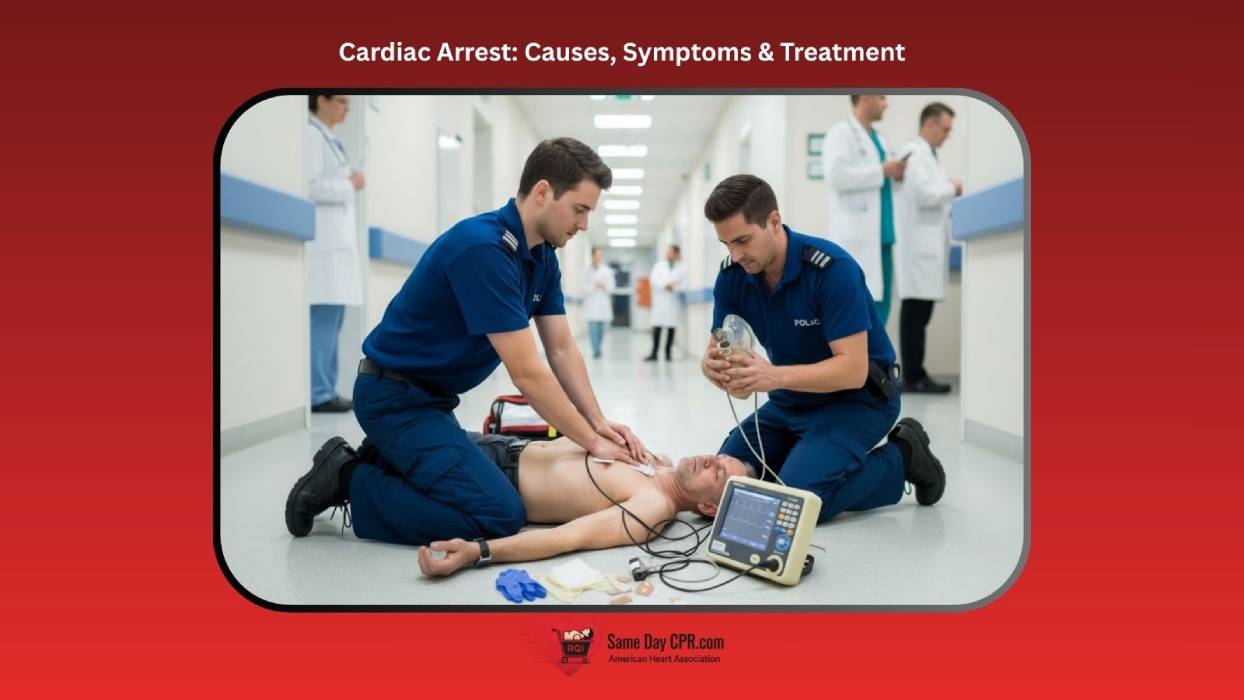
Immediate Management: BLS, ACLS, and the Chain of Survival
Cardiac arrest is a sudden, life-threatening event where the heart stops pumping effectively, leading to loss of circulation and oxygen delivery to vital organs. Survival depends on immediate recognition and intervention. The management of cardiac arrest follows structured protocols: Basic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS), both of which align with the American Heart Association (AHA) Chain of Survival.
1. Chain of Survival
The Chain of Survival is a series of critical actions that, when performed in sequence, improve the chances of survival and recovery after cardiac arrest. There are two main versions, one for out-of-hospital cardiac arrest (OHCA) and one for in-hospital cardiac arrest (IHCA).
1. Out-of-Hospital Cardiac Arrest (OHCA)
- Identify cardiac arrest quickly and call for help (911 or emergency response system).
- Begin CPR immediately with minimal interruptions.
- Use an AED (automated external defibrillator) as soon as possible to correct shockable rhythms (VF or pulseless VT).
- Provide airway management, medications, and cardiac monitoring.
- Optimize ventilation, hemodynamics, and targeted temperature management.
Also, Read: Why Are Women Less Likely to Receive Bystander CPR and AED
2. In-Hospital Cardiac Arrest (IHCA)
- Recognize patients at risk and intervene early.
- Call (911) for help at the first signs of deterioration.
- Start compressions (CPR) and defibrillate without delay.
- Continue ACLS interventions and identify reversible causes.
- Provide comprehensive care to improve neurological and cardiovascular outcomes.
2. Basic Life Support (BLS)
BLS (basic life support) focuses on maintaining circulation and oxygenation through early CPR and defibrillation. It can be performed by healthcare providers and trained lay rescuers.
Key Steps in Adult BLS
- Check Responsiveness and Breathing: Tap and shout, “Are you okay? If unresponsive and not breathing normally, call for help and get an AED.
- Activate the Emergency Response System: If alone, use a mobile phone to call 911 and put it on speaker mode. If in a hospital, call the emergency team or code blue.
- Check for a Pulse (≤10 Seconds): Palpate the carotid pulse. If no pulse → start chest compressions immediately.
- Start High-Quality CPR
- Rate: 100–120 compressions per minute
- Depth: At least 2 inches (5 cm)
- Allow full chest recoil and minimize interruptions
- Ratio: 30 compressions to 2 breaths (if trained to give rescue breaths)
- Use an AED as soon as Available: Turn it on, follow voice prompts, and deliver shock if indicated. Resume CPR immediately after shock delivery.
3. Advanced Cardiac Life Support (ACLS)
ACLS (advanced cardiovascular support) builds upon BLS by integrating advanced airway management, cardiac rhythm interpretation, medication administration, and identification of reversible causes.
Key Components of ACLS
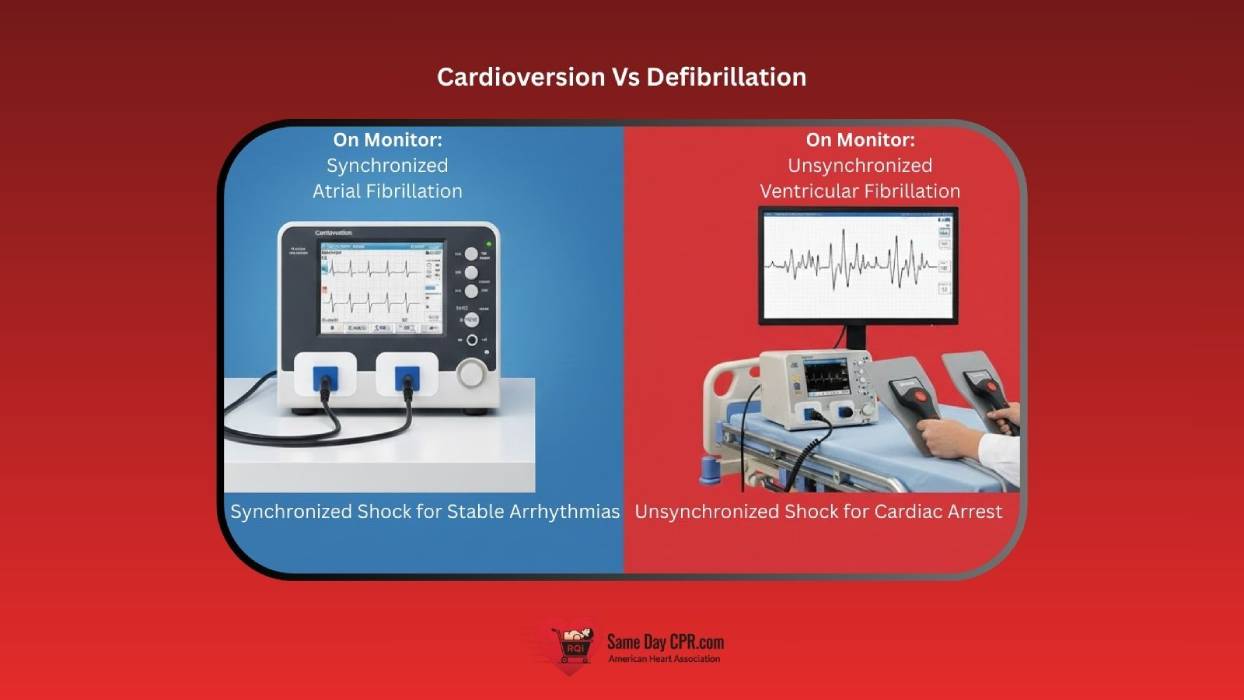
- CPR and Defibrillation
- High-quality CPR ensures continuous circulation of oxygenated blood to vital organs during cardiac arrest.
- Early defibrillation rapidly restores a shockable rhythm, significantly improving the chance of survival.
- Airway and Breathing
- Consider an advanced airway (ET tube or supraglottic device).
- Provide 1 breath every 6 seconds once an advanced airway is in place (no pauses for compressions).
- Circulation
- Administer epinephrine 1 mg IV/IO every 3–5 minutes for non-shockable rhythms (asystole/PEA).
- Administer amiodarone or lidocaine for refractory VF/pulseless VT.
- Identify and treat reversible causes (H’s and T’s)
- Hypoxia, Hypovolemia, Hydrogen ion (acidosis), Hypo-/Hyperkalemia, Hypothermia
- Tension pneumothorax, Tamponade (cardiac), Toxins, Thrombosis (pulmonary or coronary)
Also, Read: Reversible Causes of Cardiac Arrest H’s and T’s
Post-Cardiac Arrest Care
Post-cardiac arrest care is all about giving the body and brain the best chance to recover after the heart starts beating again. Once the person is stable, care continues in the ICU with close monitoring of vital signs, breathing, and blood pressure. The medical team works to protect the brain by keeping the body temperature controlled and ensuring enough oxygen reaches all organs. It’s also important to find out what caused the cardiac arrest to prevent it from happening again. This stage requires teamwork, patience, and careful attention to every small detail to help the person heal and regain strength.
Also, Read: Immediate Post-Cardiac Arrest Care Algorithm
Outcomes and Prognosis
Outcomes and prognosis after a cardiac arrest can vary widely, depending on how quickly treatment is started and the person’s overall health. Some people recover fully, while others may face lasting challenges with memory, movement, or daily activities. Doctors look at factors like age, the cause of the arrest, and how long the brain went without oxygen to estimate recovery chances. Early care, ongoing therapy, and support from family can all make a big difference in long-term recovery and quality of life.
Summary / Key Takeaways
In summary, cardiac arrest is sudden, serious, and can happen to anyone, but knowing the causes, warning signs, and how to act makes a huge difference. Quick recognition and immediate action, like starting CPR or using an AED, can save lives. Understanding the heart’s rhythms, the underlying risks, and the steps of BLS and ACLS helps both professionals and bystanders respond with confidence. Post-arrest care and ongoing support are equally important, giving the person the best chance to recover fully. Staying informed, prepared, and aware empowers you to act fast and make a real difference when every second counts.